Abstract
Background: The quality of life (QOL) of HCT patients and their caregivers declines steeply with worsening depression during the first 8 days following stem cell infusion (SCI) (El Jawahri et al, Cancer 121;951, 2015). In view of this, unique opportunities to develop programs in the confined environment of HHH to prevent the observed decrease in the QOL and address the depression of the patients and caregivers exist. The aim of this study was to gather pilot data evaluating if staying in a HHH, with its different environment and support systems and programs, has a positive impact on the QOL and mood of HCT patients and their caregivers.
Methods: This protocol was approved by the Mayo Clinic IRB and verbal consent was obtained on all participants. Patients scheduled to undergo a HCT and their caregivers were identified and asked to participate in the study. Participants completed research QOL questionnaires (LASA, FACT-G, FACT-BMT, SF-12, HADS, PHQ-8, and PROMIS) at the following time points: 15 days (+/- 15 days) prior to transplant, 1 day (+/-1 day) after SCI, 8 days (+/- 2 days) after SCI, and 30 days (+/- 7 days) after SCI. The pre-defined primary endpoint was differences in overall QOL of patients and their caregivers staying at a HHH vs. hotel, as measured by the single-item LASA.
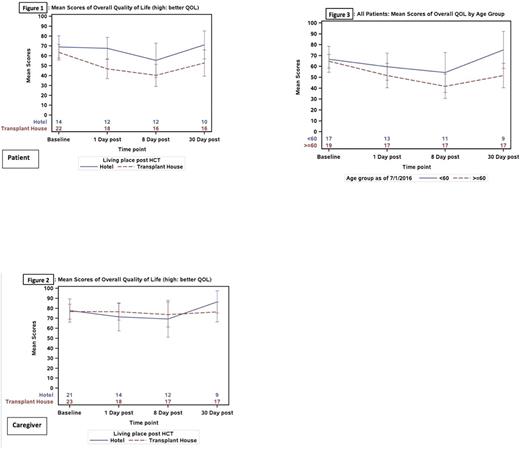
Results: A total of 44 patients and 44 caregivers were enrolled in this study from July 2016 through January 2017. Twenty-two patients completed all QOL questionnaires at all 4 time points (9 Hotel, 13 HHH) and 5 patients did not complete any QOL questionnaires (4 Hotel, 1 HHH). Day 1 post SCIQOL was worse in the HHH patients (mean = 46.9 vs. 67.6, p=0.0069, higher=better) (Figure 1); whereas, caregivers showed no significant difference in overall QOL between the living place post SCI (Figure 2). Patients who stayed at HHH were older (median age=63.2 vs. 55.4 years old, p=0.0279) and 61% of the patients were male versus 90% of the patients who stayed at hotel (p=0.0290).A multivariate analysis showed that the time point of questionnaire administration had the greatest effect on the overall QOL of patients, with day 8 post-transplant showing the most significant worsening in QOL of patients (~20 points, p=0.0006) after adjusting for other baseline characteristics. The QOL results of caregivers showed no significant difference based on place of stay; however, the data showed a tendency to favor the HHH subset. A review of data from the entire cohort of patients revealed that older patients (age >60) reported a significantly lower QOL at day 30 post HCT (mean score 51.6 vs. 75.3, p=0.0170) and lower QOL at other time points (Figure 3). There was a weak positive correlation in QOL between patient and caregiver over time except at baseline, with a correlation coefficient=0.3566.
Conclusions: Patients' age and type of HCT significantly influence patients' QOL likely accounting for the observed worse QOL of patients in the HHH subset. Living arrangements do not have a significant impact on caregivers' QOL. Additional research focusing on interventions aimed at improving the QOL and mood of HCT patients older than 60 will be of interest.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal